Pelvic Pain Symptoms, Causes, Treatment and Relief
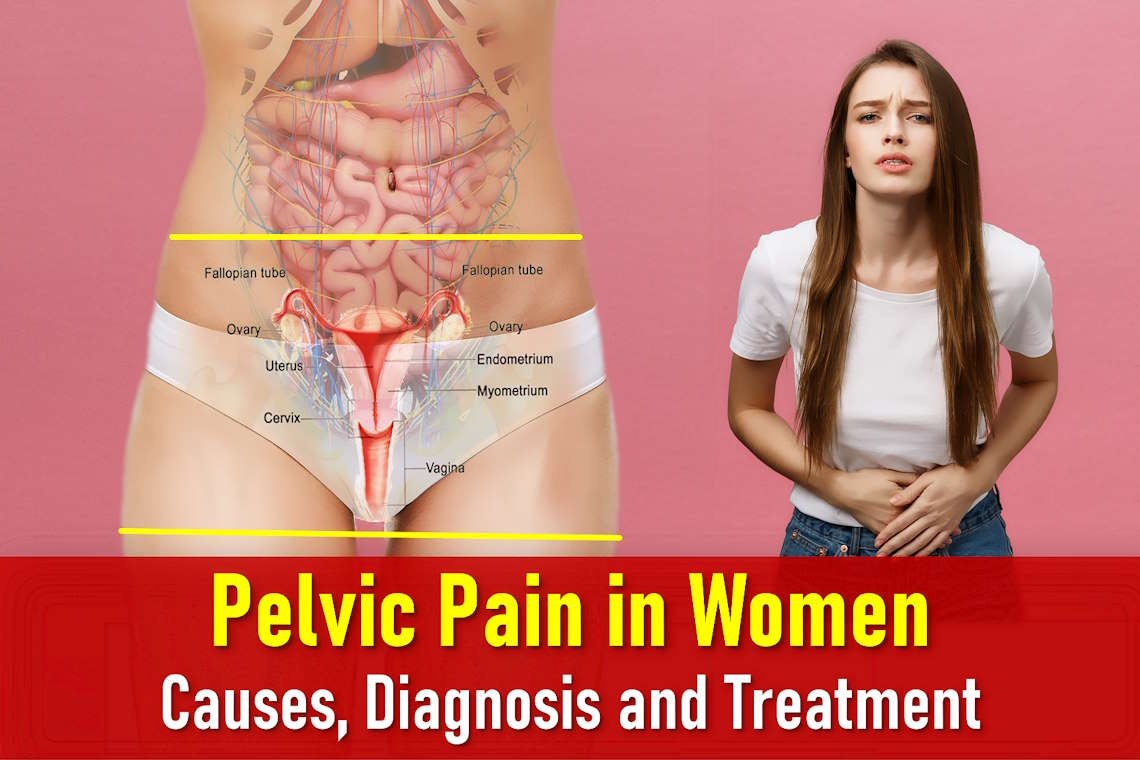
What is pelvic pain?
Pelvic pain is a common problem among women, often characterized by its varying nature and intensity. Its origins can be complex, and in some cases, no clear underlying disease can be identified. Pelvic pain can be classified as either acute, marked by sudden and severe pain, or chronic, persisting for months or longer with no significant improvement despite treatment efforts. Chronic pelvic pain, lasting over six months and unresponsive to treatment, is a distinct medical concern. This pain can have origins in pelvic organs, nerve irritation, muscle contractions, or even psychological factors, which can exacerbate or even trigger sensations of pain when no apparent physical issue exists.
Pelvic Pain Causes 
Pelvic pain may have multiple causes, including:
- Inflammation or direct nerve irritation resulting from injuries, fibrosis, pressure, or intra-abdominal inflammation.
- Contractions or cramps in both smooth and skeletal muscles.
- Common sources of acute pelvic pain, which occurs suddenly, may include:
- Ruptured Ectopic pregnancy (pregnancy outside the uterus)
- Pelvic inflammatory disease (also called PID, an infection affecting the reproductive organs)
- Miscarriage or threatened miscarriage
- Twisted or ruptured ovarian cyst
- Urinary tract infection and complication or urinary tract calculi or obstruction.
- Appendicitis and its complications
- Complications involving uterine fibroids
Causes of Chronic Pelvic Pain
Chronic pelvic pain often arises from a complex interplay of physical, psychological, and social factors rather than being attributed to a singular underlying condition. In many cases, the exact cause is unknown. Potential contributing factors include:
- Endometriosis This condition involves the presence of endometrial cells (lining of the womb) outside the uterus, primarily in the pelvic region. Both endometriosis and adenomyosis (when endometrial tissue grows into the uterine muscle) can lead to pain during menstruation and sexual intercourse.
- Pelvic Inflammatory Disease (PID) PID is an infection that affects the fallopian tubes and pelvic area, causing discomfort and pain.
- Interstitial Cystitis This condition involves inflammation of the bladder, which can result in pelvic discomfort.
- Adhesions Scar tissue formation, often stemming from prior infections, endometriosis, or surgeries, can lead to pelvic pain.
- Nerve-related Issues Pelvic pain can arise from trapped or damaged nerves within the pelvic region.
- Pelvic Organ Prolapse The descent of pelvic organs from their normal positions can cause discomfort.
- Uterine Fibroids These abnormal growths in or on the uterine wall can contribute to pelvic pain.
- Musculoskeletal Pain Discomfort originating from joints, muscles, ligaments, and bones in the pelvic area may be a source of chronic pelvic pain.
- Irritable Bowel Syndrome (IBS) IBS, a gastrointestinal condition, can produce pelvic discomfort as a symptom.
- Depression Psychological factors, including conditions like postnatal depression, can exacerbate or contribute to chronic pelvic pain.
- Traumatic Experiences Past traumatic events such as sexual or physical abuse may manifest as chronic pelvic pain.
It’s important to recognize that chronic pelvic pain is a multifaceted issue often necessitating a comprehensive assessment and tailored treatment approach to address its various components.
Pelvic Pain During pregnancy
Pelvic pain during pregnancy can result from the natural adjustments the body undergoes to accommodate the growing fetus. These changes involve shifts in bones and stretching of ligaments. Typically, this type of discomfort presents as occasional sharp or cramp-like sensations, similar to menstrual cramps, and tends to come and go. In most cases, mild and intermittent pelvic pain is considered a normal part of pregnancy and doesn’t raise concerns.
However, it’s crucial to distinguish between normal discomfort and pain that may be indicative of a pregnancy complication. Pain associated with a pregnancy-related issue may be accompanied by other worrisome symptoms, such as vaginal bleeding. Any instances of bleeding during pregnancy should prompt immediate contact with a healthcare provider. In certain conditions, this bleeding can be severe and even lead to dangerously low blood pressure (a state known as shock).
Furthermore, if a pregnant individual experiences severe, persistent pain located in the middle or upper abdomen, it could be attributed to a pregnancy complication or another underlying medical condition. In such cases, it’s essential to promptly seek medical attention and consult with a healthcare professional.
Pelvic Pain Symptoms
The following are examples of the different types of pelvic pain most commonly described by women, and their possible cause or origin. Always talk with your healthcare provider for a diagnosis.
| TYPE OF PAIN | POSSIBLE CAUSE |
|---|---|
| Localized pain | May be due to inflammation |
| Cramping | Can be caused by spasm in a soft organ, such as the intestine, ureter, or appendix |
| Sudden onset of pain | Can be caused by temporary deficiency of blood supply due to an obstruction in the circulation of blood |
| Slowly-developing pain | Could be associated with inflammation of the appendix/pelvic organs or an intestinal obstruction |
| Pain involving the entire abdomen | May suggest leakage and accumulation of blood, pus, or intestinal contents in the abdominal cavity |
| Pain aggravated by movement or during an exam | Could result from irritation in the abdominal cavity lining |
Pelvic Pain Diagnoses
The diagnosis of pelvic pain typically involves a combination of tests and inquiries into the nature of the pain. Healthcare providers may ask questions regarding:
- The timing and location of the pain.
- Duration of pain episodes.
- Any relation between pain and menstrual cycles, urination, or sexual activity.
- Pain description (sharp or dull).
- Circumstances surrounding the onset of pain.
- Rate of pain onset.
Additional information, such as the timing of pain in relation to activities like eating, sleeping, sexual activity, and movement, can also aid in the diagnosis process.
In addition to a thorough medical history and physical and pelvic exams, various tests may be required, such as blood tests, urinalysis, and imaging techniques like X-rays, ultrasounds, computed tomography (CT) scans, magnetic resonance imaging (MRI) and minimally invasive procedures like laparoscopy, hysteroscopy, cystoscopy, colonoscopy, or sigmoidoscopy.
Pelvic Pain Treatment
The specific treatment for pelvic pain depends on the underlying cause, and will be discussed with you by your healthcare provider based on:
- Your overall health and medical history
- Cause of the condition
- Onset, extent, severity, duration and progression of condition
- Your tolerance for specific medicines, procedures or therapies
- Expectations for the course of the condition
- Your opinion or preference
Treatment may include:
- Antibiotics to address infections.
- Anti-inflammatory and pain medications.
- Relaxation exercises to alleviate muscle tension.
- Oral contraceptives for hormone-related pain.
- Surgical procedures to address structural issues.
- Physical therapy to improve muscle function and alleviate pain.
- Counseling for managing chronic pain without a discernible physical cause.
- Multidisciplinary approaches, combining various strategies like nutritional modifications, environmental changes, physical therapy, and pain management techniques.
If a physical cause can’t be found, your healthcare provider may refer you for counseling to help you better cope with chronic pain. In other cases, healthcare providers may recommend a multidisciplinary treatment using a number of different approaches, including nutritional modifications, environmental changes, physical therapy, and pain management.
Treatment for Chronic Pelvic Pain
your doctor thinks that your pain is due to a particular cause then you should be offered treatment for that condition. For irritable bowel syndrome (IBS) – medication and changes to your diet may help. Infections should be treated with antibiotics. If your pain is related to your periods, you may be offered hormone treatment, for example the pill, injections or the Mirena IUS (hormone coil) to stop your periods for 3–6 months, instead of having a laparoscopy – these treatments may also be worth trying even if there is no pattern to your pain. Surgery for mild adhesions does not appear to help pelvic pain – however, it may be considered in cases of severe adhesions caused by endometriosis or previous surgery. Many women find that they can cope better with the pain if they have been listened to, taken seriously, have a full explanation of their test results and agree a plan of action. You may be reassured by finding that nothing is seriously wrong and the pain may get better with time. Some women find acupuncture or complementary therapies, or changing diet, helpful. Whatever your situation, you should be offered pain relief. If this does not help, you may be referred to a pain management team or a specialist pain clinic. Chronic pelvic pain can be very difficult to live with and can cause emotional, social and economic difficulties. You may experience depression, difficulty sleeping and disruption to your daily routine. Talk to your GP if this is the case. The support of other women who also experience pelvic pain may also help.
Frequently Asked Questions And Answers
How do you check pelvic pain?
A pelvic exam may be used to diagnose your problem. But the doctor may want to do an imaging test like a transvaginal ultrasound, a CT scan, or an MRI scan of the abdomen and pelvis for a more complete picture.
How do you know if pelvic pain is serious?
While not all pelvic pain is serious, seeking medical care when symptoms are so severe that they disrupt your daily life. You should head to the nearest emergency room if:
- Pelvic pain is sharp, severe or sudden.
- You’re unable to stand up straight.
- There’s blood in your pee or poop.
- You’re running a fever.
- You’re pregnant or have been pregnant in the last six months.
Can stress cause pelvic pain?
Even slight amounts of stress can trigger pelvic pain symptoms. Studies have shown that myofascial trigger points that are found in sore and painful muscles inside the pelvic floor are strongly affected by stress.
Can hormones cause pelvic pain?
In pelvic congestion syndrome, the veins in the pelvis are unusually dilated and engorged, causing pelvic pressure and pain. This has been shown to be related to high levels of estrogen, as estrogen causes veins to dilate. There are often other signs of hormone imbalance, such as heavy and painful periods.
What nerves cause pelvic pain?
Pudendal neuralgia (or pudendal nerve entrapment) is when you experience chronic pelvic pain from damage or irritation to your pudendal nerve. If you have pudendal neuralgia, this nerve is injured or compressed and causes stabbing, burning or shooting pain.
How can I treat pelvic pain at home?
If you have chronic pelvic pain, there are a few things you can do to ease symptoms at home:
- Take over-the-counter pain relievers. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen sodium can help reduce swelling that leads to pelvic pain. Acetaminophen can also ease painful symptoms.
- Make time for exercise. Even though you may not feel like moving, exercise helps increase blood flow and may help reduce your discomfort.
- Apply heat. Place a heating pad or warm compress over the area, or take a long soak in a hot bath.
- Stop smoking. Tobacco products can inflame nerves and cause pain. Avoiding these habits can help relieve pain.
- Take supplements. If your pelvic pain symptoms are due to vitamin or mineral deficiency, supplements could help soothe your discomfort. Talk to your healthcare provider before incorporating supplements into your daily routine.
- Practice relaxation exercises. Yoga, mindfulness or meditation can help reduce stress and tension. As a result, chronic pain may be eased.
What stage of pregnancy does pelvic pain start?
The pain may range from a mild ache to severe pain that limits your daily activities. This may start at any time during pregnancy, labour or in the weeks after giving birth . Women often feel that Pelvic Girdle Pain (PGP) affects their daily life, and that their emotional and mental health can suffer
Can pelvic pain during pregnancy affect the baby?
It can occur normally as the bones and ligaments shift and stretch to accommodate the fetus. Normal pain may be sharp or crampy (like menstrual cramps) and may come and go. Usually, pelvic pain that is not severe or persistent is not a cause for concern.
Does pelvic pain in pregnancy cause miscarriage?
Pelvic pain in early pregnancy may also be caused by miscarriage. The most serious cause of pelvic pain in early pregnancy is an ectopic pregnancy, which is pregnancy that occurs outside the uterus. Ectopic pregnancies require immediate medical attention.
Key Points About Pelvic Pain
Pelvic pain is a common issue among women, characterized by its varying nature and potential causes. It can be acute or chronic, with treatment options ranging from medications and physical therapy to surgery and counseling. Identifying the precise cause of pelvic pain is essential for tailoring an effective treatment plan that addresses the root of the issue. If you experience persistent pelvic pain, consult with a healthcare provider to determine the most appropriate course of action.