Painless Delivery ( Epidural injection )
What Is a Painless Delivery (Epidural Analgesia)?
Epidural analgesia, often referred to as a painless or epidural block, is a widely used medical procedure during labor and childbirth. It is considered one of the most effective methods for alleviating pain during this transformative experience. In fact, more than half of individuals giving birth in hospital settings opt for epidural analgesia to manage the discomfort associated with labor and delivery.
Understanding Epidural Analgesia
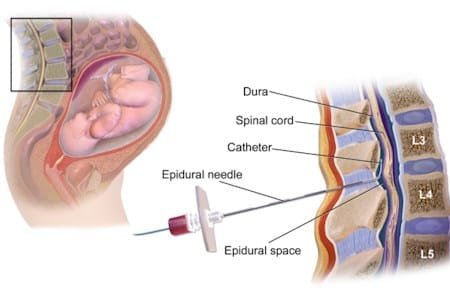
An epidural is a specialized medical intervention designed to provide pain relief to individuals during the labor and delivery process. It derives its name from the “epidural space,” a region outside the spinal cord where the medication is delivered. This procedure involves the introduction of anesthetic agents and pain-relieving medications through a thin, flexible tube called a catheter. By carefully controlling the administration of these medications, healthcare providers can effectively numb the sensation of pain, making the experience of childbirth significantly more manageable for the laboring individual.
Types of Epidurals
There are two primary types of epidurals commonly used during labor and childbirth:
- Epidural with a Catheter: In this method, the healthcare provider administers medication through a catheter inserted into the lower back via an epidural injection. The catheter remains in the epidural space, allowing for the adjustment of medication dosage as needed.
- Combined Spinal-Epidural (CSE): A Combined Spinal-Epidural (CSE) is a unique approach that combines two distinct injections: a spinal injection (spinal block) and an epidural. This combination offers rapid pain relief, and because it typically involves a lower medication dose, it allows for more sensation in the lower body. This increased sensation enables the individual to move more freely and change positions. The CSE approach is sometimes referred to as a “walking” epidural, although full mobility is often limited.
Epidural Anesthesia vs. Epidural Analgesia
It’s important to distinguish between epidural analgesia and epidural anesthesia : –
- Epidural Analgesia: This approach offers pain relief without causing unconsciousness or complete loss of sensation. It is commonly used during labor and delivery to manage pain caused by contractions and childbirth. –
- Epidural Anesthesia: Epidural anesthesia, on the other hand, can temporarily numb the spinal nerves, resulting in the loss of physical sensation. While it does not induce unconsciousness, it may be used in certain surgical procedures to ensure the individual does not feel pain or move during surgery.
Advantages of Painless Delivery
The decision to opt for epidural analgesia during labor and childbirth is a personal one, and individuals should carefully consider their preferences and consult with their healthcare providers. Understanding the advantages of epidural analgesia can aid in making an informed choice: –
- Effective Pain Relief: Epidurals are highly effective at alleviating the pain associated with labor and delivery, providing individuals with a sense of comfort during this challenging process.
- Safety: Epidurals are generally considered safe when administered by trained healthcare professionals. Serious complications are rare.
- Mobility and Control: Epidurals often allow individuals to maintain some mobility, enabling them to shift positions in bed and push when necessary.
- Rest and Recovery: For those experiencing prolonged labor, epidurals can provide a respite, allowing individuals to rest and regain their strength. –
- Suitable for Various Situations: In the event of a Cesarean section (C-section), individuals with epidurals can remain awake and alert during the procedure, and their partners can typically be present as well. –
- Flexible Timing: Epidurals can generally be administered at any stage of labor, providing flexibility for individuals to make this choice when it aligns with their needs and preferences.
The Epidural Procedure
The administration of an epidural begins with a thorough consultation between the expectant individual and the healthcare provider. During this discussion, the healthcare team will address any concerns, answer questions, and provide detailed information about the procedure.
- Preparation: Before the epidural procedure, a healthcare provider will likely insert a cannula into a vein in the arm. This cannula allows for the attachment of an intravenous (IV) line, which can be used if necessary to stabilize blood pressure during the epidural.
- Patient Positioning: The individual receiving the epidural is typically positioned either sitting upright or lying on their side. This positioning allows for proper access to the epidural space in the lower back.
- Sterile Procedure: The healthcare provider ensures a sterile environment by cleansing the skin in the lower back area with an antiseptic solution. This meticulous preparation minimizes the risk of infection.
- Local Anesthesia: To minimize discomfort during the procedure, the healthcare provider may inject a local anesthetic into the skin and deeper tissues of the lower back. This can cause a brief sensation of burning or pressure.
- Epidural Placement: The critical step in the procedure involves advancing a needle into the epidural space, which is situated outside the dural sac that contains the spinal cord and cerebrospinal fluid. Once the needle is in the correct position, a small catheter is threaded through it and placed precisely in the epidural space. The needle is then removed, leaving the catheter in place.
- Medication Infusion: The catheter serves as a conduit for the infusion of anesthetic and pain-relieving medications. This steady flow ensures sustained pain relief throughout labor and delivery.
- Monitoring: During an epidural procedure, your health will be closely watched to make sure you and your baby are safe. This means keeping a close eye on important signs like your blood pressure and oxygen levels. It’s essential to note that because of this monitoring, you might not be able to move around as freely.
- Delivery: When your cervix is fully dilated, your midwife will let you know when it’s time to push. You’ll be encouraged to push during contractions. The epidural will continue until after your baby is born, the placenta is delivered, and any necessary stitching is done.
Additional Facts About Epidurals
Here’s what you should know about epidurals:
- Epidurals don’t typically make the first stage of labor longer or increase your chances of a C-section.
- However, they can make the second stage of labor longer, which might lead to a forceps or vacuum-assisted birth.
- The good news is that epidurals usually don’t cause long-term backache.
- If you choose an epidural, expect more monitoring, including frequent blood pressure checks and an IV drip. Your baby’s heartbeat will also be closely watched with electronic monitoring for the first 30 minutes after the epidural and after each top-up.
- Your epidural should be given in a way that allows you to move a bit initially, but as you get top-ups during labor, your mobility may decrease. Some epidurals can be topped up by you.
Risks of Epidural ( Painless Delivery )
Epidurals are generally safe and provide relief from pain and discomfort during childbirth. Serious complications are very rare, but like any medical procedure, there are potential side effects:
- Your blood pressure may briefly drop, affecting your baby’s heart rate. To prevent this, you’ll receive fluids through an IV.
- If your blood pressure drops, lying on your side and medication can help stabilize it.
- Epidurals may make your legs feel heavy due to the local anesthesia used.
- Limited mobility during labor, which can make changing positions or standing difficult until the medication wears off.
- Difficulty pushing and possibly a longer second stage of labor.
- Difficulty feeling contractions and pushing, increasing the chance of instrumental delivery with forceps or vacuum.
- Possible challenges if the baby is in an abnormal position.
- Temporary difficulty urinating, which may require a catheter.
- Occasional headache, which can be treated.
- Soreness in your lower back where the needle was inserted, typically lasting a few days.
- Rarely, tingling or pins and needles in one leg.
- Extremely rare cases of dizziness, breathing difficulty, or seizures if medicine enters the spinal fluid.
Remember that the benefits of pain relief often outweigh the potential risks, and your healthcare team will closely monitor you throughout the process to ensure a safe and comfortable childbirth experience.
Frequently Asked Questions about Epidurals
Does Epidural Slow Labor or Lead to C-Section?
A common concern among expectant individuals is whether epidurals slow down the progress of labor or increase the likelihood of a C-section. Research and medical consensus indicate that epidurals do not typically impede labor progress or contribute to a higher likelihood of a Cesarean section. The decision to perform a C-section is typically influenced by various factors, including the size or position of the baby and the progression of labor.
Can Epidurals Harm the Baby?
Another important consideration for expectant parents is the potential impact of epidurals on the baby. It’s natural to prioritize the safety and well-being of both the laboring individual and the baby. Fortunately, epidurals are designed with safety in mind. The amount of medication that reaches the baby from the epidural is minimal, and there is no evidence to suggest that it causes harm to the baby.
Can Epidurals Cause Back Problems?
There is a commonly held belief that receiving an epidural during labor can lead to long-term or chronic back problems. However, this notion is largely unfounded. While it is normal to experience temporary soreness or tenderness at the site of the epidural injection, this discomfort typically resolves within a few days. It’s essential to recognize that the post-childbirth period often involves various physical adjustments, including the repositioning of bones and ligaments in the pelvis, which can contribute to back pain and discomfort.
When is an Epidural for Labor Pain Administered?
The timing of when to initiate an epidural during labor is a matter of personal choice. Expectant individuals have the flexibility to request an epidural at any stage of labor. However, it is commonly recommended to wait until the active labor phase begins, as epidurals are most effective during this stage when contractions are more intense.
Does it Hurt When the Epidural is Administered?
One common question individuals have is whether the epidural procedure itself is painful. To minimize discomfort during the administration of an epidural, healthcare providers typically employ a two-step process:
- Local Anesthesia: Before the epidural injection, a local anesthetic is often used to numb the skin and deeper tissues in the lower back. This can cause a brief stinging or burning sensation.
- Epidural Injection: Following the application of local anesthesia, the epidural needle is inserted. During this step, you may feel pressure, tingling, or a momentary sensation of discomfort. However, the level of pain experienced is usually minimal, and any discomfort tends to subside once the injection is complete.
What Does an Epidural Do?
Epidurals serve a crucial role in labor and childbirth by providing anesthesia that creates a “band” of numbness extending from the belly button to the upper legs. Importantly, this method allows individuals to remain awake and alert throughout the labor process while still being able to perceive pressure and sensations. The ability to feel the pressure associated with the second stage of labor is vital as it enables individuals to push effectively during the birth of their baby. It’s worth noting that it typically takes around 15 minutes for the pain medication to take full effect.
How Long Does the Pain Relief Last?
Epidurals offer sustained pain relief throughout labor and delivery. The duration of pain relief can be extended or reduced by adjusting the dosage of medication delivered through the epidural. This flexibility allows healthcare providers to tailor the pain management approach to the individual’s specific needs.
Do Doctors Recommend Epidurals?
The decision to opt for an epidural is a personal one and should align with an individual’s preferences and medical needs. Healthcare providers are valuable sources of information and guidance in this decision-making process. There are situations in which healthcare providers may recommend epidurals, particularly when labor pain is exceptionally intense, leading to exhaustion or a sense of loss of control. Additionally, having an epidural in place can expedite pain management if a Cesarean section becomes necessary.
Is Painless Delivery Good for Pregnancy?
Research and clinical experience have demonstrated that epidurals are safe and effective for the vast majority of individuals undergoing labor. However, it’s important to recognize that the choice of pain relief method during childbirth is a personal one. Expectant individuals deserve access to accurate information to make informed decisions that align with their health, pregnancy, and personal preferences.
When Is the Best Time to Get an Epidural?
The optimal time to request an epidural is a matter of individual preference. While it can be requested at any stage of labor, it’s essential to be aware that epidurals may take up to 15 minutes to provide full pain relief. In active labor, when contractions are intense, a combined spinal-epidural (CSE) technique may be considered for more immediate relief.
Who Shouldn’t Get a Painless Delivery?
While epidurals are a suitable pain relief option for many, certain medical conditions or circumstances may preclude individuals from receiving an epidural. It’s crucial to engage in open and transparent communication with your healthcare provider to discuss your medical history and address any concerns. Conditions such as allergies to anesthetic drugs, blood clotting issues, or active infections may influence the decision to use an alternative pain relief method.