Laparoscopic Hysterectomy, Procedure, Benefits, Risks and Recovery
A laparoscopic hysterectomy is a minimally invasive surgical procedure performed under general anesthesia to remove the uterus (womb). This common surgical intervention can also involve the removal of the fallopian tubes, ovaries, and cervix to address various gynecological issues.
Why Is a Laparoscopic Hysterectomy Necessary ?
A laparoscopic hysterectomy is typically considered a last resort when other treatments have proven ineffective, unless it’s required to address conditions like cancer. The decision to undergo a hysterectomy should be a collaborative one between you and your doctor. In most cases, a laparoscopic hysterectomy becomes necessary to alleviate acute or chronic painful and distressing symptoms, especially when other treatment options have failed. The primary goal of this procedure is to resolve these symptoms and improve your quality of life. Here are some reasons why a laparoscopic hysterectomy might be recommended:
- Heavy or Painful Periods When all other treatment options have been explored and heavy or painful periods significantly affect your quality of life, a laparoscopic hysterectomy may be considered. Sometimes, severe anemia may develop as a result of heavy uncontrolled bleeding.
- Fibroids are benign (non-cancerous) growths or tumors, typically found in the muscular wall of the uterus. They can vary in size and position and may cause heavy and painful periods. Large fibroids can also press on the bladder, leading to urinary symptoms.
- Adenomyosis is a condition where the uterine lining grows into the muscular wall of the uterus, often occurring alongside endometriosis and sharing similar symptoms
- Endometriosis occurs when the lining of the uterus (endometrium) is found outside the uterus, often on the fallopian tubes, ovaries, and other nearby organs like the bladder or bowel. This misplaced tissue can cause lower abdominal pain, scarring, and pain during intercourse.
- Cancer A laparoscopic hysterectomy may be advised if you develop cancer of the uterine lining. Your doctor or oncology nurse can provide more information about cancer treatment.
Types of Laparoscopic Hysterectomy

There are different types of laparoscopic hysterectomy, including:
- Total Hysterectomy Removal of both the uterus and cervix.
- Subtotal Hysterectomy (Supracervical Hysterectomy) Removal of the uterus while leaving the cervix intact.
- Bilateral Salpingo-Oophorectomy (BSO) with hysterectomy: Combined removal of one or both ovaries and fallopian tubes performed alongside the above procedures.
- Total Laparoscopic Radical Hysterectomy Removal of the entire womb, cervix, fallopian tubes, ovaries, and support structures , blood vessels and lymph nodes around these structures along with part of the vagina, , typically for cancer treatment.
What to Expect Before the Procedure
Before the surgery, you will have a pre-operative assessment where a nurse will explain your hospital stay and details of the operation. Make any necessary arrangements for your family or childcare before coming to the hospital. You will meet with the anesthetist and the surgeon who will perform the operation. It’s normal to feel anxious, and the nursing staff is there to address your concerns and emotions.
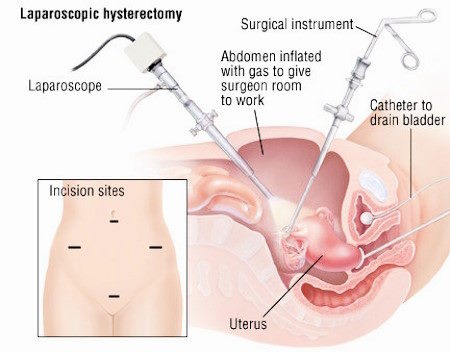
The Laparoscopic Hysterectomy Procedure
During a laparoscopic hysterectomy, small incisions are made in the abdomen, which is why it’s often referred to as “keyhole surgery.” Special surgical instruments are inserted through these incisions, and the procedure is conducted using an internal telescope and camera system. The uterus is removed through the vagina, and other tissues, including lymph nodes, may be removed either through the vagina or small abdominal incisions. Typically, two to four small scars, each measuring 0.5 cm to 1 cm, remain on different parts of the abdomen. If the cervix is removed, there will also be a scar at the top of the vagina, out of sight.
Risks of Laparoscopic Hysterectomy
As with any surgical procedure, there are risks associated with laparoscopic hysterectomy. These risks include:
Common Risks
- Postoperative pain, particularly shoulder tip pain.
- Urinary infection, retention, or frequency.
- Wound infection, bruising, and delayed wound healing.
Uncommon Risks
- Damage to the bladder.
- Damage to the bowel.
- Pelvic abscess or infection.
- Venous thrombosis and pulmonary embolism (clot in leg/lung).
- Failure to gain entry to the abdominal cavity and complete the procedure.
- Hernia at the site of entry.
- Hemorrhage requiring blood transfusion.
- Return to the operating room due to bleeding.
- Unexpected laparotomy (abdominal incision).
- Vaginal vault dehiscence (opening) requiring re-suturing.
Before undergoing the surgery, it’s essential to discuss any questions or concerns with your healthcare team. You will need to sign a consent form to demonstrate your informed choice.
Recovery from Laparoscopic Hysterectomy
After the surgery, as you wake from anesthesia, you may experience episodes of pain and/or nausea. Inform the nursing staff if you do, and they will assess and address your discomfort. Your vital signs will be monitored, and you will be encouraged to move to prevent complications like deep vein thrombosis (DVT), or chest infections.
You will have a catheter to drain urine, which will be removed the following morning. Expect pain and discomfort in your lower abdomen during the first few days after the operation. You may also experience shoulder tip pain due to trapped gas and water, which is common with laparoscopic surgery. Pain medication will be provided.
You will have 2-4 small dressings on the incisions in your abdomen, which are waterproof and allow you to shower and maintain hygiene. Blood thinning injections may be administered to prevent DVT.
Other post-operative care include:
- Resting during the first two weeks, gradually increasing daily activities.
- Expecting some vaginal discharge/bleeding for 1-2 weeks.
- Monitoring stitches, which are usually dissolvable.
- Taking measures to prevent DVT.
- Engaging in light household activities initially and gradually increasing intensity.
- Gradually reintroducing exercise, such as walking.
- Maintaining a balanced, high-fiber diet and staying hydrated.
- Considering the resumption of sexual activity after 2-4 weeks.
- Planning for a 2-6 week recovery period before returning to work.
- Evaluating your readiness to drive, typically after 3-6 weeks.
Alternatives to Laparoscopic Hysterectomy
If you prefer not to undergo surgery, there are alternative methods to address your symptoms, such as hormone preparations like an intrauterine system, endometrial ablation (a procedure to destroy the uterine lining), or pharmacological therapies. Discuss these options with your doctor.
Frequently Asked Questions (FAQs) about Laparoscopic Hysterectomy
What are the advantages of laparoscopic hysterectomy over traditional surgery?
The advantages include smaller incisions,less complications, quicker recovery , reduced post-operative pain, less need of pain killer medications and minimal scarring compared to traditional open surgery.
How long does a laparoscopic hysterectomy surgery typically take?
The surgery typically takes anywhere from 1 to 3 hours, depending on the complexity of the case and the surgeon’s experience.
What is the recovery time for a laparoscopic hysterectomy?
Recovery times vary, but most women can return to light activities within a few weeks and resume normal activities within 4 to 6 weeks.
Are there any risks associated with laparoscopic hysterectomy?
While laparoscopic hysterectomy is generally safe, there are risks, including infection, bleeding, injury to surrounding organs, and anesthesia-related complications. Your surgeon will discuss these risks with you.
Will I experience menopause after a hysterectomy?
If your ovaries are removed during the hysterectomy (oophorectomy), you may experience menopause symptoms. If the ovaries are preserved, menopause will occur naturally when your ovaries stop producing hormones.
Can I still have children after a laparoscopic hysterectomy?
No, a hysterectomy removes the uterus, making intrauterine pregnancy impossible. However, if your ovaries are preserved, pregnancy at other locations in the abdomen is a possibility ,although very rare.
What should I expect during the recovery period?
During recovery, you should expect some discomfort and pain, possible vaginal bleeding, and restrictions on lifting heavy objects. Follow your surgeon’s post-operative instructions closely.
How can I prepare for a laparoscopic hysterectomy?
Pre-operative preparation typically involves taking leave from work, overnight fasting before surgery, discontinuing certain medications, and arranging for transportation home after the being discharged from hospital.
Is laparoscopic hysterectomy covered by insurance?
Most health insurance plans cover medically necessary hysterectomies, but it’s essential to check with your insurance provider and your surgeon’s office to understand your specific coverage and potential out-of-pocket costs.
What alternatives are there to laparoscopic hysterectomy?
Alternative treatments may include medications, hormone therapy, myomectomy (removal of fibroids), or other minimal endoscopic surgical options as well as traditional open procedures . The choice depends on your specific condition and preferences.
Can I choose to keep my ovaries during the procedure?
Yes, you can discuss with your surgeon whether it’s possible to preserve your ovaries, depending on your medical condition and individual health goals.
How experienced is my surgeon with laparoscopic hysterectomies?
It’s crucial to ask your surgeon about their experience with laparoscopic procedures and their success rate to ensure you are in capable hands.
Are there any dietary or lifestyle changes I should make before surgery?
Your surgeon may recommend specific dietary or lifestyle changes before surgery to optimize your health and improve the success of the procedure. Follow their guidance closely.







