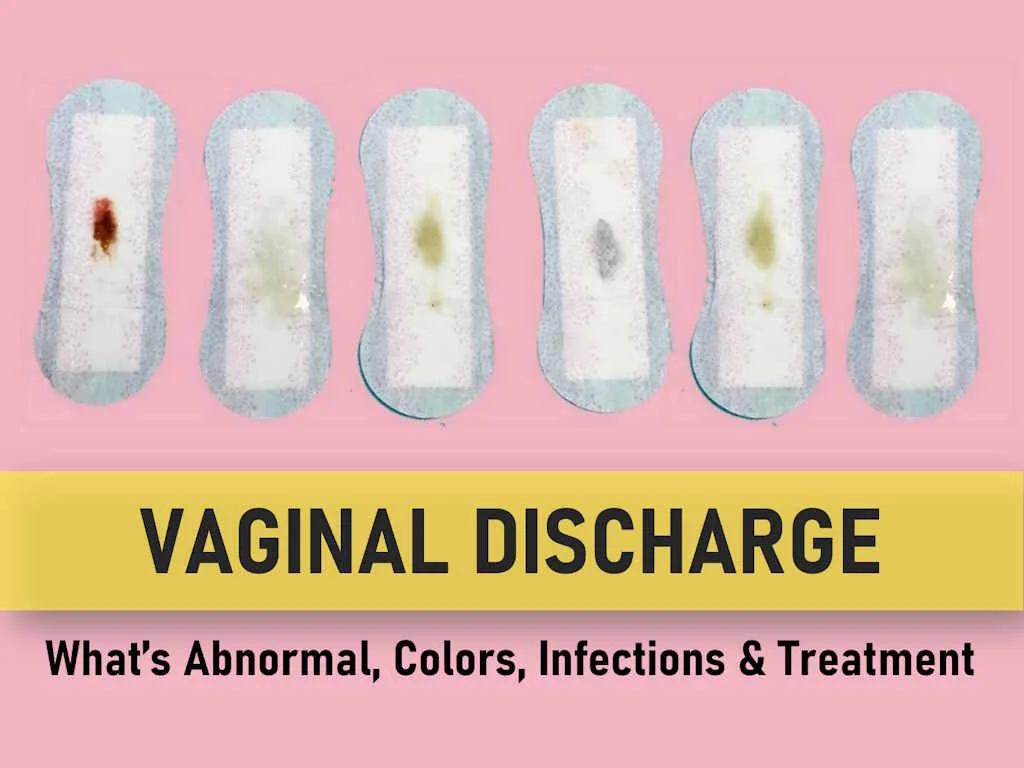
Vaginal Discharge: What’s Abnormal, Colors, Infections & Treatment
Vaginal discharge refers to the fluid or mucus that emanates from the vagina. Typically, this discharge comprises vaginal skin cells, bacteria, mucus and fluids produced by the vagina and cervix. Vaginal discharge is a common concern for women and often prompts them to seek medical advice. While a certain amount of vaginal discharge is considered normal, it becomes concerning when accompanied by itching, burning, or other discomforting symptoms.
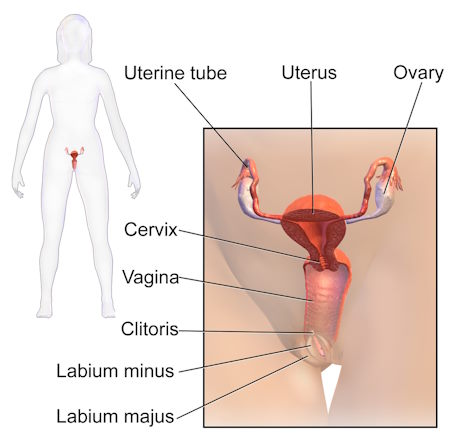
Understanding Female Anatomy
Before understanding the intricacies of vaginal discharge, it’s essential to grasp the fundamentals of female reproductive anatomy. Vaginal discharge is generally inconspicuous until it exits the vagina, which serves as the conduit from the uterus to the external body. At the upper end (inside) of the vagina resides the cervix, while the lower end (outside) leads to the vulva and labia. The vulva is the skin surrounding the vaginal opening. Numerous glands within the cervix and vagina continually produce secretions and mucus to maintain the vaginal walls well-lubricated and clean. This mucus plays a crucial role in vaginal cleanliness and is home to both beneficial and harmful bacteria. When a specific type of bacteria over proliferates, infections can ensue.
Normal Vaginal Discharge
Vaginal discharge is primarily a product of the cells lining the vagina and cervix, influenced by the female hormone estrogen. Menopausal women typically experience minimal vaginal discharge due to lower estrogen levels. In reproductive age women, a daily output of roughly one-half to one teaspoon (2 to 5 mL) of white or clear, thin, mucus-like, mostly odorless vaginal discharge is considered normal. Its consistency can resemble that of egg whites, though the amount and texture may vary between individuals and throughout the menstrual cycle. Some individuals may produce more discharge than others. Occasionally, vaginal discharge may carry an odor, but it should not be overpowering or unpleasant. Factors such as hormonal fluctuations during pregnancy, ovulation, or the use of hormonal birth control methods can lead to heightened discharge. Additionally, sexual arousal can trigger increased production from vulvar glands.
Vaginal Discharge Colors and What They Mean
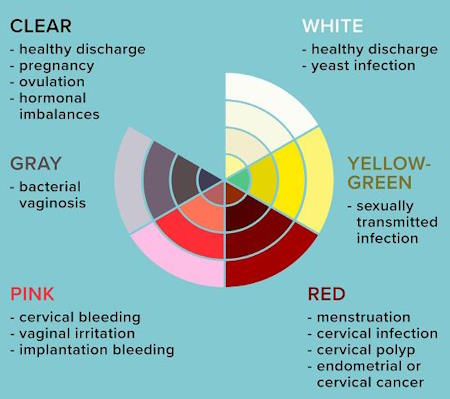
Vaginal discharge varies in color and consistency and is influenced by factors such as age, behaviors, menstrual cycle, and other symptoms. Understanding what each color might indicate is essential for identifying normal versus abnormal discharge.
Yellow Vaginal Discharge
Yellow vaginal discharge can be normal but becomes concerning when it is:
- Thick
- Chunky
- Smelly
This type of discharge may indicate a trichomoniasis infection, which is often sexually transmitted, especially if the discharge is yellow-greenish. Chlamydia or gonorrhea, although frequently asymptomatic, can also cause yellow discharge in some women.
Yellow Vaginal Discharge After Sex
A thick, chunky, or foul-smelling yellow discharge after sex, especially if accompanied by itching, suggests a sexually transmitted infection (STI) such as trichomoniasis, gonorrhea, or chlamydia. Human papillomavirus (HPV) infections usually result in a bloody, brown, or watery discharge with an odor.
Green Vaginal Discharge
Green vaginal discharge is typically abnormal and indicative of an infection. A thick, chunky, and foul-smelling green discharge often suggests a sexually transmitted disease like trichomoniasis.
White Vaginal Discharge
A small amount of white discharge, particularly at the start or end of your menstrual cycle, is normal. However, if the discharge is accompanied by itching and has a thick, cottage cheese-like consistency, it may indicate a vaginal yeast infection. A milky white discharge could also suggest bacterial vaginosis or an sexually transmitted infection (STI) if it is accompanied by symptoms such as odor or pelvic pain.
Clear and Watery Vaginal Discharge
A clear and watery discharge is normal and can occur at any time during the month. It may be particularly heavy after physical exercise.
Brown Vaginal Discharge
Brown discharge during menstruation or towards the end of a period is usually normal. Late discharge at the end of your period can appear brown instead of red, often due to old blood leaving the body. If spotting occurs at the expected time of your period and you had unprotected sex, it might indicate pregnancy. Brown discharge or spotting during early pregnancy can also be a sign of a miscarriage, so seeing a doctor is advisable.
Brown Vaginal Discharge Post-Menopause
Postmenopausal brown discharge could be concerning and may indicate potential cancer of the female organs, including advanced cervical cancer. It’s crucial to have regular pelvic exams and Pap smears to check for cervical abnormalities.
Pink Vaginal Discharge
Pink vaginal discharge is often associated with premenstrual spotting or early pregnancy implantation bleeding. Some individuals may experience spotting after ovulation or sexual intercourse due to minor vaginal irritation.
Causes of Abnormal Vaginal Discharge
Various factors can disrupt the pH balance of a healthy vagina, including douching, feminine hygiene products, specific soaps or bubble baths, and the use of broad-spectrum antibiotics. Pregnant women and those with diabetes are at higher risk of infections. Common causes of abnormal vaginal discharge include:
- Vaginal Infections (yeast, bacterial, trichomonas, and sexually transmitted infections).
- Body’s Reaction to Foreign Bodies or Irritants (such as forgotten tampons, condoms, or allergic reactions to detergents, soaps, lubricants, or materials used in sex toys).
- Menopausal Changes Resulting in Vaginal Dryness (atrophic vaginitis).
- Uterine Infections (e.g., pelvic inflammatory disease).
- Uterine or Cervical Cancer (may manifest as foul-smelling blood-stained discharge).
- Vaginal and Vulval Skin Disorders (leading to abnormal discharge).
Potential Causes of Infective Vaginal Discharges
Several infections can lead to changes in vaginal discharge or unpleasant odors, often transmitted through sexual contact:
- Yeast Infection. Characterized by overgrowth of the Candida fungus, resulting in thick, white, cottage cheese-like discharge, itching, and discomfort.
- Trichomoniasis or “Trich”. A sexually transmitted infection caused by a parasite, leading to green, yellow, or gray, bubbly or frothy discharge.
- Bacterial Vaginosis (BV). Occurs when certain bacteria overpopulate the vagina, causing white or gray, foul-smelling, fishy discharge.
- Gonorrhea and Chlamydia. Common sexually transmitted infections that can cause cloudy, yellow, or green vaginal discharge if left untreated, potentially leading to complications such as pelvic inflammatory disease and urinary infections.
When to Seek Medical Attention
A change in vaginal discharge color, consistency, or odor may indicate an infection, warranting evaluation by a healthcare provider. Following are the Signs to be aware of:
- Thick, white vaginal discharge.
- Altered appearance of usual discharge.
- Vulvar itching or irritation.
- Redness, burning, soreness, swelling, blisters, bumps, or sores on the vulvar skin.
- Foamy or greenish-yellow discharge.
- Foul odor (e.g., Fishy odor of bacterial vaginosis).
- Blood-tinged vaginal discharge.
- Pain during intercourse or urination.
- Abdominal or pelvic pain.
Examination for Vaginal Discharge
Determining whether vaginal discharge is normal or abnormal typically requires a physical examination and laboratory testing of a vaginal specimen. Self-diagnosis and home treatment should be avoided, as they can complicate accurate diagnosis. Relying on internet or social media recommendations is also discouraged. Before the examination, your healthcare provider may inquire about:
- Any pain in your back, abdomen, or pelvis.
- Recent changes in sexual partners.
- Menstrual cycle history.
- Medication usage (including prescription, herbal, and nonprescription drugs).
- Use of pads, tampons, douches, feminine hygiene products, lubricants, pH-altering treatments, or boric acid.
- Diabetes or other chronic illnesses.
- Experiences of pain during urination or sexual activity.
During the examination, the healthcare provider will conduct a comprehensive assessment of the outer genital area and perform an internal examination. A sample of the discharge will be collected for infection testing, with attention to measuring its pH, as bacterial vaginosis and trichomoniasis can elevate pH levels.
High-Risk Factors for Abnormal Vaginal Discharge
Certain practices and characteristics increase the likelihood of developing abnormal vaginal discharge, such as individuals who:
- Use douches.
- Regularly use pantyliners.
- Employ “feminine hygiene” sprays, powders, or rinses.
- Engage in bubble baths or use scented bath products.
- Wear tight or synthetic clothing.
- have unprotected sex or have multiple sexual partners.
- Have untreated or poorly managed diabetes.
- Use birth control pills.
- Are prescribed antibiotics.
- Have HIV infection or a compromised immune system.
Healthier Practices to Prevent Abnormal Vaginal Discharge
To reduce the risk of vaginal infections and abnormal discharge, consider the following practices:
- Regularly shower or bathe using mild soap or water; avoid using bubble bath.
- Refrain from using vaginal sprays and scented products.
- Use plain white toilet tissue.
- Always wipe from front to back after visiting the bathroom.
- Wash hands before touching the vaginal area.
- Use unscented non-soap cleanser with warm (not hot) water and the hand (not a washcloth) to cleanse the genitalia.
- Urinate after intercourse to help prevent urinary tract infections.
- Use unscented tampons, sanitary pads, and liners; change them every 2 to 3 hours.
- Remove tampons before bedtime and use pads instead.
- Avoid douching or using feminine hygiene products; consult a healthcare provider if odor or discharge is bothersome.
- Opt for cotton or cotton-lined undergarments for better moisture absorption; avoid tight-fitting synthetic clothing, leggings, tights, or pants that inhibit airflow.
- Maintain a healthy lifestyle through proper nutrition, regular exercise, and sufficient sleep.
- Limit the number of sexual partners and use condoms to prevent sexually transmitted infections.
- Adhere to prescribed medication regimens, and if recommended by a healthcare provider, lose weight if weight-related issues contribute to infections.
- Notify sexual partners if you have a sexually transmitted infection for proper evaluation and treatment.
Vaginal Discharge Treatment
Treatment for abnormal vaginal discharge varies based on the underlying cause. Diagnosis and treatment should ideally follow a physical examination and rapid bedside laboratory tests. In some cases, treatment may be delayed until further test results are available. It’s crucial to note that not all vaginal symptoms stem from infections.
If treatment is prescribed by a clinician, it’s essential to understand the test results and the type of infection present. Sexual partners of individuals with sexually transmitted infections, such as chlamydia, gonorrhea, or trichomoniasis, should also seek evaluation and treatment. In contrast, for infections like yeast or bacterial vaginosis, sexual partners typically do not require treatment.
It is advisable to abstain from intercourse until treatment is completed. While abnormal vaginal discharge is treatable, it can recur, and in such cases, consultation with a healthcare provider is essential for potential extended treatment.
Treatment for Specific Infections:
- Yeast Infections. Typically treated with antifungal medications administered vaginally. Individuals who experience frequent yeast infections may be advised to use preventive treatment alongside antifungal medication.
- Bacterial Vaginosis. Treated with oral/vaginal antibiotics.
- Trichomoniasis: Usually managed with oral antibiotics.
- Sexually Transmitted Infections (STIs). These can be more challenging to treat and are easily transmitted. All sexual partners should be informed and treated simultaneously, and sexual activity should be avoided until both you and your partner are infection-free.
Frequently Asked Questions about Vaginal Discharge
Why does Vaginal Discharge smell like Vinegar?
Vaginal discharge with a tangy, sharp, or acidic scent, resembling vinegar, is usually a sign of a healthy vagina maintaining a normal pH balance. This smell is caused by the presence of beneficial bacteria, called lactobacilli, which help protect the vagina by preventing the growth of harmful bacteria that can lead to infections.
Should I douche to eliminate vaginal discharge?
No, douching should not be used to eliminate vaginal discharge. Douching can disrupt the body’s natural balance of organisms and may lead to infections. Normal vaginal discharge is a natural and healthy process, and it is not unclean or harmful. It serves to maintain vaginal cleanliness and health by removing fluids and old cells.
Can I self-treat the vaginal discharge using home remedies?
While many women may prefer to avoid visiting a healthcare provider, self-treatment can delay an accurate diagnosis, incur unnecessary costs, or exacerbate symptoms. In most cases, a physical examination should precede any treatment. Douching or using boric acid vaginal capsules should be avoided, as they can worsen discharge and potentially spread infections to the uterus and pelvis.
How does vaginal discharge change during pregnancy?
During pregnancy, it is normal to experience an increase in the volume of vaginal discharge. This change is designed to prevent infections from ascending into the uterus. Elevated levels of progesterone can also contribute to increased discharge. If you notice any unusual changes in vaginal discharge during pregnancy, consult your prenatal care provider for guidance.
Why does my vaginal discharge have a smell?
An unpleasant or strong “fishy” odor associated with vaginal discharge could indicate an infection. A foul-smelling discharge may indicate a bacterial infection or neglected foreign body such as a tampon.
Is yellow vaginal discharge with no odor normal?
Yellow vaginal discharge without a strong odor is generally considered normal, especially if it’s light and doesn’t cause discomfort. However, if it becomes thick or chunky, it could indicate an infection such as bacterial vaginosis or trichomoniasis, which should be evaluated by a healthcare provider.
Is it normal to have clear vaginal discharge after stopping birth control?
Yes, it is common to notice clear vaginal discharge after stopping birth control as your hormones begin to regulate. This type of discharge can indicate that your body is resuming its natural menstrual cycle, including ovulation. If the discharge has an unusual color or smell, or is accompanied by discomfort, consult your doctor.
What causes clear vaginal discharge after a hysterectomy?
Clear vaginal discharge after a hysterectomy is usually normal and part of the healing process, particularly in the weeks following surgery. If the discharge becomes foul-smelling or bloody, it could indicate an infection, and you should contact your healthcare provider.
Is clear vaginal discharge after ovulation normal?
Clear vaginal discharge after ovulation is normal and usually occurs because of increased estrogen levels. The discharge may resemble egg whites and is a natural sign of fertility. It helps in making the environment in the vagina more suitable for sperm.
Why do I experience clear vaginal discharge after sex?
Clear vaginal discharge after sex is typically due to natural lubrication produced during intercourse. This type of discharge can also help cleanse the vagina of any foreign matter. If the discharge has a strong odor or unusual color, it may signal an infection.
What does clear vaginal discharge after a miscarriage indicate?
Clear vaginal discharge after a miscarriage is generally part of the body’s healing process. However, if the discharge is accompanied by a foul odor, fever, or abdominal pain, it could suggest an infection, and you should seek medical attention.
Is it normal to have vaginal discharge after a hysterectomy?
Some level of vaginal discharge after a hysterectomy is expected, especially during the initial recovery period. However, if the discharge is excessive, has an unusual color, or is accompanied by pain or fever, it could indicate complications that require medical attention.
Can vaginal discharge be a sign of herpes?
Yes, vaginal discharge can be a symptom of herpes. If you have a herpes infection, you might notice an increase in vaginal discharge, along with painful sores or blisters in the genital area. If you suspect you have herpes, it’s important to get tested and receive appropriate treatment.
Summary
Vaginal discharge, a clear, white, or off-white fluid originating from the vagina, is a natural and regular bodily process. It consists mainly of cells, gland secretions, and bacteria, serving to cleanse and lubricate the vagina while combating harmful bacteria and infections. While variations in discharge are common, changes in color, texture, smell, or volume may signify underlying issues. Most causes of abnormal vaginal discharge are treatable, and an annual visit to a healthcare provider is essential for sexually active individuals. Finally, observing vaginal hygiene and few lifestyle adjustments go a long way in prevention of abnormal vaginal discharge.