Acne Causes and Treatment
Acne is a skin condition in which the pores become blocked, causing pimples to develop. Acne stands out as the most prevalent skin disorder in North America, impacting around 85 percent of adolescents. There are effective treatments accessible to address existing pimples and prevent the development of new ones. In addition, cosmetic treatments can help to reduce scarring and changes in skin color caused by acne.
How does acne develop ?
There are four basic steps involved in the development of an acne lesion.
- Hair follicles become blocked with an overabundance of normal skin cells (figure 2). These cells mix with sebum, an oily substance that lubricates the hair and skin, forming a plug in the follicle.
- The glands that produce sebum, known as sebaceous glands, enlarge during adolescence and sebum production increases (figure 3). Numerous sebaceous glands are found on the face, neck, chest, upper back, and upper arms.
- The increase in sebum production allows for the overgrowth of bacteria that normally lives on the skin.
- Bacterial overgrowth causes local inflammation, which causes rupture of the follicle (figure 4). This may result in the development of a red or tender pimple.
The basic acne lesion is called a comedo. The most common types of pimples are:
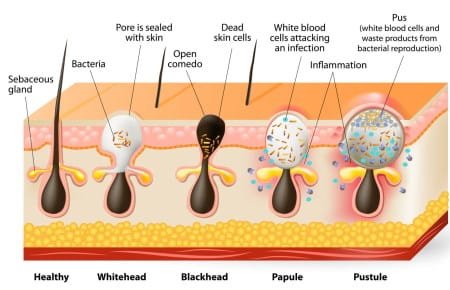
- Whiteheads (closed comedones): Small, closed bumps with a white appearance, formed when a hair follicle is clogged with oil and skin cells.
- Blackheads (open comedones): Pimples with a small, black opening at the top, caused by the oxidation of sebum exposed to air.
- Papules: Tender, small pink bumps on the skin’s surface, often indicating inflamed pores.
- Pustules: Inflammatory acne characterized by pimples with pus on the top and a red base.
- Nodules: Hard, large, and painful pimples that develop deep within the skin.
- Cysts: Deep, painful, pus-filled pimples that can result in scarring, representing a severe form of acne.
Acne causes
- Hormonal changes. Hormonal changes during adolescence cause the sebaceous glands to become enlarged and sebum production increases. In most people with acne, hormone levels are normal, but the sebaceous glands are highly sensitive to the hormones. Less often, women’s hormone levels are affected by an underlying medical problem known as polycystic ovary syndrome (PCOS). Acne tends to resolve between ages 30 to 40, although it can persist into or develop for the first time during adulthood. Post-adolescent acne predominantly affects women, in contrast to adolescent acne, which predominantly affects men. Acne can flare before a woman’s menstrual period, especially in women older than 30 years.
- External factors. Oil-based cosmetics may contribute to the development of acne. Oils and greases in hair products can also worsen skin lesions. Water-based or “non-comedogenic” products are less likely to worsen acne. People with acne often use soaps and astringents. While these treatments remove sebum from the skin surface, they do not decrease sebum production; frequent or aggressive scrubbing with these agents can actually worsen acne.
- Diet. The role of diet in acne is controversial. Some studies have found weak associations between cow’s milk and an increased risk of acne, perhaps because of hormones that occur naturally in milk. However, there is no strong evidence that milk, high-fat foods or chocolate increase the risk of acne.
- Stress. Psychological stress can probably worsen acne. In several studies of students, acne severity appeared to worsen during times of increased stress.
- Medicines. Certain medicines, such as those used to treat epilepsy and types of depression.
- Pressure or friction on the skin. Friction caused by backpacks or bike helmets can make acne worse.
- Family history. If other people in your family have acne, there is a greater chance you will have it.
What can you do to reduce acne?
The way you take care of your skin has a big effect on your acne. Here’s what you should do:
- Skin Hygiene: Wash your face no more than twice daily using a gentle non-soap facial cleanser with warm (not hot) water. Some providers recommend using hands instead of a washcloth or loofah to wash the face to avoid irritation. Vigorous washing or scrubbing can exacerbate acne and harm the skin’s surface. Avoid picking or squeezing pimples to prevent worsening acne, skin swelling, scarring, and the risk of infection.
- Moisturizers: Use moisturizer to minimize dryness and peeling, which are common side effects of certain acne treatments. Use products labeled as “non-comedogenic” to reduce the likelihood of blocking skin pores.
- Sun Protection: As some acne treatments heighten sensitivity to sunlight (e.g., retinoids, doxycycline), protect your skin by avoiding excessive sun exposure and applying sunscreen with SPF 15 or higher before going out.
- Makeup and Hair Care: Choose makeup and hair care products labeled “non-comedogenic” or “non-acnegenic” to avoid acne-inducing ingredients. Use oil-free products to further reduce the risk.
- Skin Friction: Minimize activities that rub against the skin, such as using backpacks or sports equipment, to prevent irritation.
- Medical Consultation: Discuss treatment options with your doctor to determine the most effective approach for your acne. Take prescribed medications as directed, and inform your doctor if any other medications worsen your acne.
Can I treat my own acne?
If you have mild acne, consider non-prescription products initially. Salicylic acid, benzoyl peroxide, sulfur, alpha hydroxy acids, or tea tree oil are available in non-prescription strengths. Combining these treatments may enhance effectiveness. If there’s no improvement after three months or if you have moderate or severe acne, consult a healthcare provider for personalized advice on more effective treatments.
Acne treatment
There is no single best treatment for acne, and healthcare providers may suggest combinations of treatments. Since acne lesions typically take at least eight weeks to mature, you should use a treatment for a minimum of two to three months before assessing its effectiveness.
Noninflammatory acne
Noninflammatory acne causes whiteheads or blackheads without redness or skin swelling .
Retinoids. Topical retinoid medications are often recommended for noninflammatory acne. Examples of these medications include tretinoin, adapalene and tazarotene. Retinoids are typically administered once daily, and those experiencing skin irritation can adjust the frequency to every other day or less, gradually increasing as tolerated. With time, most individuals develop increased tolerance to retinoids. These formulations are commonly available in gel or cream forms, with gels being preferred by those with oily skin due to their drying effect, while individuals with dry skin may opt for creams. It’s important to note that retinoids may lead to skin irritation, and during their use, applying a sunscreen with SPF 15 or higher before sun exposure is recommended.
Other acne products. Individuals who cannot tolerate retinoids may consider other topical medications, such as salicylic acid, glycolic acid, or azelaic acid. All of these treatments can be helpful in reducing noninflammatory acne, and azelaic acid may reduce acne-related darkening of skin.
Mild to moderate inflammatory acne
Mild to moderate acne with some inflammation (picture 2) is usually treated with topical retinoids, topical antibiotics, or benzoyl peroxide. A combination of two medications, usually benzoyl peroxide with a topical antibiotic or retinoid (eg, tretinoin), is more effective than treatment with one agent alone.
Moderate to severe inflammatory acne.
For individuals dealing with moderate to severe inflammatory acne, healthcare professionals may recommend oral antibiotics or an oral retinoid known as isotretinoin. Complementary use of topical medication may be advised. Women, especially, may find hormonal treatment through a birth control pill beneficial.
Acne and pregnancy
Several acne treatments are not safe for use during pregnancy. Women who are pregnant or planning to conceive should consider discontinuing all acne treatments before becoming pregnant. If acne therapy becomes essential, it is advisable to discuss the available options with your healthcare provider.











