What Is Pap Smear or Pap Test? Age Recommendations, Procedure & Results
What is a Pap Smear Test or Pap Test?
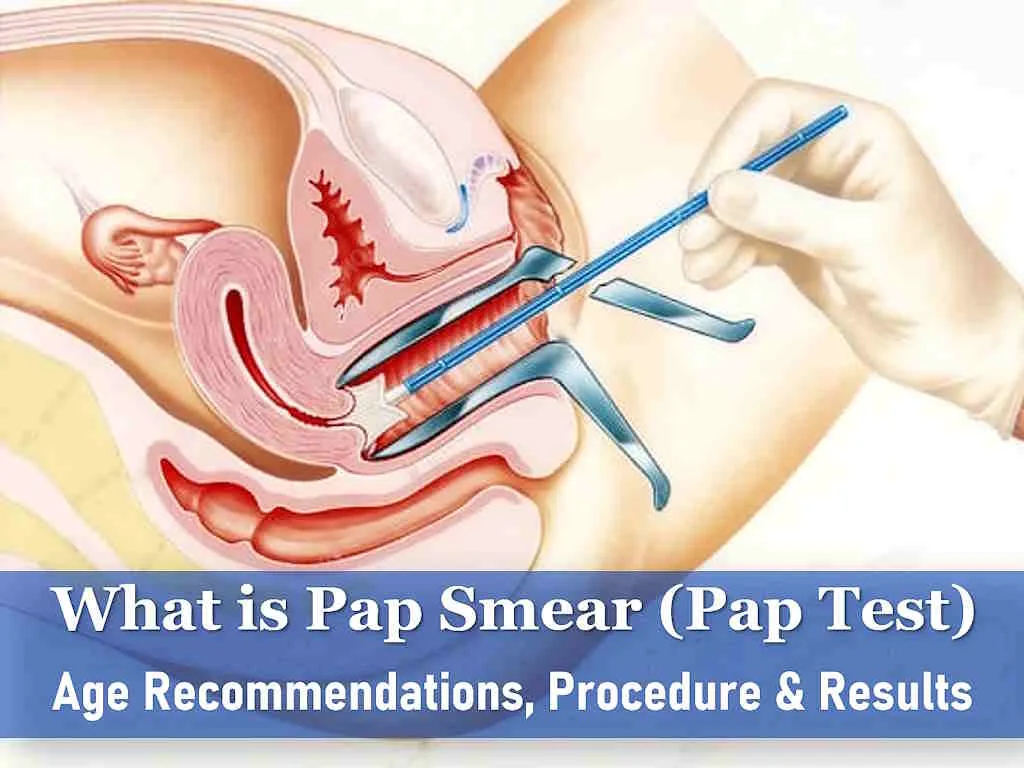
A Pap smear, also known as a Pap test, cervical cytology, Papanicolaou test, or vaginal smear technique, is a crucial women’s health screening test designed to detect or prevent cervical cancer. During this procedure, a healthcare provider collects cells from the cervix, the lower and narrow end of the uterus that opens into the vagina. These cells are then examined for cancerous or precancerous changes. Detecting and treating precancerous cells is vital for preventing cervical cancer. Pap smears are a reliable means of early cancer detection when it is most treatable. When diagnosed and addressed in its early stages, cervical cancer is not life-threatening.
What is Cervical Cancer?
 Cancer can grow on your cervix (the lower part of the uterus) the same way it can grow on other body parts. Most times, cervical cancer grows slowly. It can take about 10 to 15 years (or more) for abnormal cells to transform into cancer. cervical cancer remains asymptomatic until it reaches an advanced stage. Symptoms such as abnormal bleeding, discharge, or pain may appear in women with advanced cervical cancer. Notably, a distinctive aspect of cervical cancer is that it is predominantly instigated by a specific type of virus. When found early, cervical cancer is highly curable.
Cancer can grow on your cervix (the lower part of the uterus) the same way it can grow on other body parts. Most times, cervical cancer grows slowly. It can take about 10 to 15 years (or more) for abnormal cells to transform into cancer. cervical cancer remains asymptomatic until it reaches an advanced stage. Symptoms such as abnormal bleeding, discharge, or pain may appear in women with advanced cervical cancer. Notably, a distinctive aspect of cervical cancer is that it is predominantly instigated by a specific type of virus. When found early, cervical cancer is highly curable.
Did you know?
Cervical cancer is not hereditary like other cancers. It is the fourth most frequent cancer in women globally. There were an estimated 342,000 deaths from cervical cancer in 2020, with 90% of these occurring in middle and low-income countries. Annually in the United States, approximately 12,000 women are diagnosed with cervical cancer, and almost 4,000 women die from it. Cervical cancer is preventable through routine screening tests and timely treatment, making it the most preventable cancer among women.
Pap Smear, Age Guidelines
The CDC provides recommendations for Pap smear testing schedules based on age, as outlined below:
Ages below 21: Cervical cancer screening is not recommended for women or girls under the age of 21, as their risk of cervical cancer is extremely low, and cervical cell changes often resolve spontaneously.
Ages 21–29: Begin Pap tests at age 21. If results are normal, consider waiting 3 years until the next test.
Ages 30–65:
- Discuss with your doctor whether to have a Pap test alone or a combined Pap and HPV test.
- If having a Pap test alone and results are normal, consider waiting 3 years for the next one.
- If having a combined test with normal results, consider waiting 5 years for the next screening test.
Age 65 and Older:
- For individuals over 65, screening may no longer be necessary if:
- They have consistently had normal screening test results for many years.
- They have undergone a total hysterectomy, including cervix removal.
- However, the National Cancer Institute recommends that people over 65 continue Pap smear tests if they have specific risk factors for cervical cancer, including:
- Immunosuppression.
- Previous treatment for a precancerous cervical lesion or cervical cancer.
- Living with HIV.
- Exposure to diethylstilbestrol before birth.
Remember, If you have had a hysterectomy, you still may need screening. Women who have been vaccinated against HPV still need to follow the screening recommendations for their age group.

How the Pap Smear Test is Performed?
To perform a Pap smear test, a doctor or other health care provider will perform a pelvic exam and use a small brush or spatula to collect cells from the cervix. The collected sample of cervical cells will then be preserved and sent to a laboratory for testing to identify the presence of abnormal cells. An HPV test can be done along with a Pap test on same sample.
Pap Smear Test Results
Your Pap smear test is reported as abnormal, inconclusive or normal.
Normal: A normal or “negative” result indicates that no abnormal cell changes were detected on your cervix. While this is good news, it’s important to continue getting Pap tests in the future because new cell changes can still develop over time.
Inconclusive (also known as ASC-US): Sometimes, test results may be unclear, and your doctor might use terms like equivocal, inconclusive, or ASC-US to describe this result. These terms all essentially mean the same thing: your cervical cells appear potentially abnormal, but it’s unclear whether it’s related to HPV. Other factors, such as life changes (e.g., pregnancy, menopause, or an infection), could be influencing these changes. An HPV test can help determine if these cell changes are HPV-related.
Abnormal: An abnormal Pap smear result indicates that cell changes were detected on your cervix. However, it’s essential to understand that an abnormal result does not necessarily mean you have cervical cancer. Abnormal cervical changes are often attributed to HPV infection. These changes can be classified as minor (low-grade) or significant (high-grade). In most cases, minor changes tend to revert to normal on their own. However, more severe changes can progress to cancer if left untreated. These significant changes are often referred to as “precancerous” because they aren’t cancer yet but have the potential to develop into cancer within three to seven years. In rare instances, an abnormal Pap test might suggest the presence of cancer, but further tests are needed to confirm it. Detecting cervical cancer early makes it easier to treat.
Follow-up tests
Based on your test results, your healthcare provider may recommend the following:
- Routine testing, according to guidelines. Depending on your age and test results, this may be every 3 years or every 5 years.
- Follow-up testing with a Pap test and an HPV test in one year.
- Colposcopy: This is a procedure that involves examining the cervix using a microscope with a bright light to assess any abnormal changes more closely and taking biopsies from suspicious areas.
How to prepare for Pap Smear Test?
Generally, there is no specific preparation required for a Pap smear.
- You should schedule the test when you are not having your period, since blood can interfere with the results of the test.
- Avoid the following for at least 24 hours before having a Pap smear test:
- Sexual intercourse.
- Vaginal douching.
- Using tampons or vaginal lubricants.
- Applying vaginal creams, suppositories, or medications.
- Using birth control foam, cream, or jelly.
Do I have cervical cancer if I have HPV?
No, having HPV does not mean you have cervical cancer. HPV is the virus that can lead to cervical cancer, but not everyone with HPV develops the disease, as most of the women clear out the virus over time. Women with HPV can prevent cervical cancer by following their doctor’s recommendations for additional testing and, if necessary, treatment.
Do you need a Pap Smear if you’re not sexually active?
Yes, regular Pap smears are still recommended for individuals who are not sexually active because abnormal cell growth can occur due to factors other than sexual activity, increasing the risk of cervical cancer.
Does a Pap Smear hurt?
Pap smears aren’t painful. But sometimes, you can have a mild pain and uncomfortable feeling for a short time. Women frequently describe it as a small pinch, but everyone’s pain threshold is different. Usually the most uncomfortable part is when the speculum is opened inside the vagina, which can stretch the vaginal and vulval tissues ,leading to a pressure feeling. However, some women will find a smear test painful. There are many physical and psychological reasons that can make a smear test painful or uncomfortable. Conditions like vulvodynia, endometriosis or menopausal vaginal dryness might make the pap smear painful or uncomfortable. Sexual violence, female genital mutilation or a previous traumatic medical experience may also lead to the same outcome. If you experience pain and you want to stop, tell the doctor or nurse to do so.
Why is cervical screening painful for some women?
There are many reasons why pap smear may be painful, including: –
- Vaginismus, which means that the vagina suddenly tightens as you try to put something into it.
- Cervical ectropion or cervical erosion.
- Vaginal dryness other post-menopausal symptoms.
- Female genital mutilation (FGM), when the genital area is deliberately cut, injured or changed as in some cultures.
- Clenching, or feeling unable to relax, due to nerves, anxiety or a previous bad experience of sexual violence.
- Other gynecological issues.
How can we reduce the discomfort during pap smear?
You should let your doctor/nurse know about your concerns and any relevant conditions or experiences that could make your smear more uncomfortable or painful. You can ask to lie in a different position that’s more comfortable or use of a smaller speculum with more lubrication. You can also request to pass the speculum yourself if you are experienced in it. Try breathing exercises to help your body relax. Remember, you can ask to stop at any point if you’re feeling pain or overwhelming anxiety.
Bleeding after a pap smear test?
A little bit of bleeding and cramping after a smear test is fairly common, as the cervix is sensitive and might be irritated during the procedure. This bleeding should be very light and should stop within a few hours. If the bleeding does not stop in twenty four hours, is heavy, or you are in a lot of pain, you should contact your doctor.
Can you get a pap Smear on your Period?
The accuracy of pap smear results is impacted if it is done during periods. The presence of menstrual blood makes it challenging for your healthcare provider to obtain a clear sample of cervical cells. There will also be difficulty in reading the slides and giving reliable result. If your appointment falls during your periods, it is better to reschedule your appointment for a time when you are not menstruating. If you have spotting or light bleeding, you may be able to continue.
Is a pap smear the same as a pelvic test?
A pap smear is not the same as a pelvic exam, though it is also performed with a speculum. In a pelvic exam the doctor examines in detail the reproductive organs, including the vagina, vulva, cervix, ovaries, and uterus. During pap smear your doctor will only examine your vulva, vaginal opening and cervix for unusual discharge, redness, or other irritation and take a smear from the cervix.
Does pap smear test for chlamydia and other STIs?
Chlamydia cannot be detected through a Pap smear test. A Pap smear is a test doctors use to check if a woman has any precancerous or cancerous cells in her cervix. It is not a test for chlamydia. Each assessment may incorporate a pelvic examination, yet they obtain samples from distinct areas of the person’s reproductive passage.
Chlamydia, an STI caused by the bacterium Chlamydia trachomatis, has the potential to accumulate in the urethra, throat, and rectum. Consequently, medical professionals might extract swabs from various locations. The Centers for Disease Control and Prevention (CDC) says that doctors may take a cervical swab to test for chlamydia and scrape cervical cells for a Pap smear test if the patient wishes to be tested for chlamydia as well. Doctors may combine a Pap smear with a test for human papillomavirus (HPV), another common STI. HPV infections may become chronic, or long lasting, and increase a woman’s risk of developing cervical cancer.
The CDC recommends regular screening for cervical cancer and chlamydia. Chlamydia is diagnosed through the application of nucleic acid amplification tests (NAATs). Samples of genital fluids or urine are taken and sent to a laboratory for analysis.
Doctor / nurse can collect samples of vaginal fluids by taking a swab during a pelvic exam.
Cervical cancer is a significant health concern, leading to thousands of deaths among women annually. A Pap smear, when complemented by HPV testing, stands as one of the most effective preventive measures against the development of cervical cancer.