Intrauterine Device IUD, Types, Benefits and Side Effects
What is an IUD
An Intrauterine Device (IUD), also known as an Intrauterine Contraceptive Device (IUCD), a copper tee or multi-load coil, is a contraceptive method involving the insertion of a device into the uterus (womb) to prevent pregnancy. The IUD is a small plastic device shaped like a ‘T’ with attached plastic strings. It is one of the most effective methods of contraception. However, despite their efficacy, many women remain hesitant about considering this option. Proper understanding is essential in embracing and reaping the immense benefits of this form of contraception.
Types of IUDs
Two types of IUDs are available: – 
- The Copper IUD (also known as the non-hormonal copper IUD). The copper IUD is a small, T-shaped plastic and copper device that consistently releases a small amount of copper into the uterus. It can also serve as an alternative for emergency contraception, replacing the emergency contraceptive pill (commonly referred to as the ‘morning after pill’) if used within 5 days following unprotected intercourse.
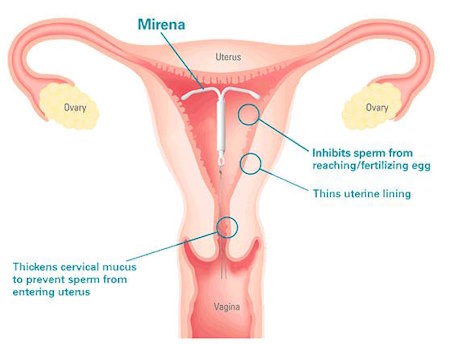
- The Hormonal IUD : hormonal IUDs release levonorgestrel, a synthetic hormone. (Mirena™ and Kyleena™). Mirena thickens cervical mucus and thins the endometrium, preventing sperm from entering the fallopian tubes. Mirena is also known to partially suppress ovulation. Kyleena is a lower-dosage variation of Mirena and has been accessible in Australia since 2020.
Both the copper IUD and hormonal IUDs are designed for extended use, with the copper IUD remaining effective for up to 10 years and hormonal IUDs (Mirena™ and Kyleena™) for 5 years. If necessary, they can be removed earlier.
IUDs, like contraceptive implants, are categorized as Long-Acting Reversible Contraception (LARC) because they provide protection against pregnancy for several years. The “long-acting” aspect implies that once inserted, it offers contraception for an extended duration, and the “reversible” nature means that its contraceptive effect fades when removed. These soft, flexible, T-shaped devices are placed within the uterus and feature two thin plastic strings extending into the vagina.
The choice between these options depends on various factors, including your preferences and specific health considerations.
Effectiveness of IUDs
Both copper and hormonal IUDs are highly effective, boasting an efficacy rate of over 99% in preventing pregnancy.
Getting an IUD
Your doctor or nurse practitioner will prescribe an IUD, which you can then obtain from a pharmacy. In some cases, you may purchase a copper IUD directly from the clinic performing the insertion. Trained medical professionals, either doctors or nurses, will perform the IUD insertion.
Monitoring and Record-Keeping
IUDs come with a fine nylon thread attached, which extends through the cervix (the opening to the uterus). By reaching high up inside your vagina, you can periodically check for the presence of this thread, ensuring the IUD remains in place. Since the thread is situated deep within the vagina, it is not visible externally. Keeping a record of the insertion date is advisable to ensure timely removal before its expiry (5 or 10 years, depending on the type).
The Mechanics of IUDs: How Do They Work?
IUDs create a mild inflammatory environment inside the uterus, rendering it unfavorable for sperm survival and impeding implantation. Hormonal IUDs further thicken cervical mucus and thin the endometrium, making it inhospitable for the implantation of a fertilized egg.
Why Choose an IUD Over Other Birth Control Methods?
IUDs offer several compelling advantages:
- Long-Acting: Most IUDs provide contraception for 3 to 10 years, offering long-term peace of mind.
- Empowerment: IUDs put the control of pregnancy prevention in a woman’s hands, allowing her to decide when to conceive.
- High Effectiveness: When correctly placed, IUDs boast an impressive 99% effectiveness rate in preventing pregnancy.
Who Is Eligible for an IUD?
Virtually any woman, whether young or old, with or without children, can be a candidate for an IUD. However, certain conditions, such as a history of infections, fibroids, or suspicions of genital malignancies, may exclude individuals from this contraceptive option.
Advantages of IUDs
- IUDs offer several advantages, including:
- Extremely high effectiveness, preventing pregnancy in over 99% of cases.
- Long-term protection, with Mirena™ and Kyleena™ lasting up to 5 years and the copper IUD up to 10 years.
- Lowering the risk of endometrial cancer
- Eliminating adverse effects associated with estrogen-based contraceptives
- Safe use while breastfeeding.
- Compatibility with most medications, unaffected by other drugs.
- Providing a suitable option for those who cannot use estrogen-based contraception (unlike combined pills and vaginal rings, which contain both estrogen and progestogen). The hormonal IUD contains only progestogen, while the copper IUD has no hormones.
- Minimal maintenance, with the need for only monthly thread checks post-period to ensure proper placement.
- Easy removal by a trained healthcare professional, with fertility quickly returning to normal once the IUD is removed.
Additional Benefits of Hormonal IUD
The hormonal IUD offers additional advantages:
- Reduced or no vaginal bleeding for most users(Mirena is indicated for heavy bleeding as a treatment).
- Potentially less painful periods.
Additional Benefits of Copper IUD
The copper IUD provides:
- A hormone-free contraceptive option.
- Effectiveness as a method of emergency contraception.
Possible Side Effects of IUDs
Possible side effects for both types of IUDs include:
- Initial period-like cramping that typically subsides within a few days.
- Occasional IUD expulsion, more common in the first 3 months post-insertion.
- Changes in your menstrual cycle. Spotting or frequent bleeding is common during the first 3 to 6 months with mirena, but around 90-95% of users may experience a light, regular period or no bleeding at all after 6 months. This is not harmful to the body.
- Occasional symptoms such as tender breasts, headaches, skin changes, and mood changes, which usually resolve with time. The hormonal IUD is not associated with weight gain.
- Copper IUDs may cause heavier and painful periods .
With Mirena ,some women can experience changes in their menstrual pattern as under:
- Can find their first period is a lot lighter but continue a lot longer
- Can experience irregular bleeding or spotting for the first 3-6 months
- 95% of women will find menstruation is a lot lighter and less painful.
- 30% of women will not have any periods as long as the Mirena is in.
Potential Health Risks of IUDs
In rare cases:
- During IUD insertion, a small hole in the uterine wall may occur in about 1 in 500 individuals. If the IUD moves through this hole and misplaces, it may necessitate keyhole surgery (laparoscopy) for removal.
- Approximately 1 in 300 people may develop an infection shortly after IUD insertion, which can be successfully treated with antibiotics.
- Although it’s unlikely to get pregnant with an IUD in place, if pregnancy does occur, there’s a higher risk of an ectopic pregnancy (where the pregnancy implants in the fallopian tubes). Seek immediate medical attention if this happens.
When an IUD May Not Be Suitable ?
An IUD might not be suitable for individuals with:
- A uterus that is not of the typical shape.
- An existing pelvic infection.
Additionally:
- The hormonal IUD may not be appropriate for individuals who have been treated for breast cancer or have severe liver disease.
- The copper IUD may not be suitable for those with heavy periods, low iron levels, or endometriosis.

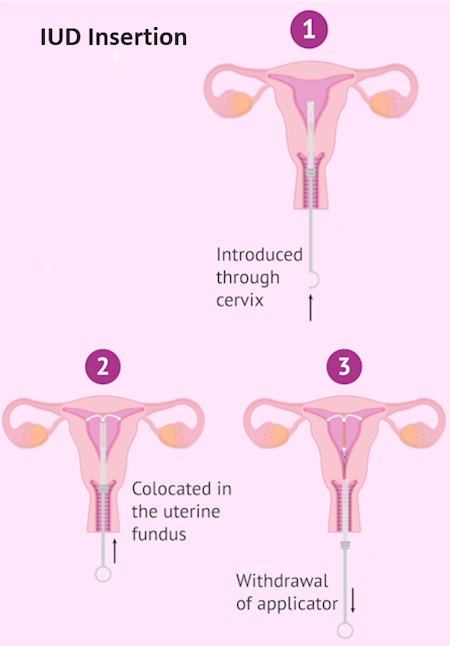
IUD Insertion Procedure
Initially, your healthcare provider, whether a nurse or doctor, will conduct a thorough medical history review, followed by an examination of your vagina, cervix, and uterus. Additionally, they might conduct testing for sexually transmitted diseases (STDs). In some cases, you may receive medication to facilitate the dilation and numbness of your cervix before the IUD insertion.
The IUD insertion procedure involves the following steps:
- Your healthcare provider will place a speculum into your vagina to gain clear access.
Using a specialized inserter, they will gently introduce the IUD through the cervical opening and into your uterus.
This entire process is typically completed in under five minutes.
Pregnancy While Using an IUD
If you become pregnant while using an IUD, consult a doctor or nurse promptly to have the IUD removed. This medical professional will also assess the possibility of an ectopic pregnancy in the fallopian tubes. If the IUD is removed, you can choose to continue or terminate the pregnancy.
Using an IUD After Childbirth
You can have an IUD inserted within 2 days after giving birth. If not inserted immediately after birth, wait at least 4 weeks. IUDs are safe to use while breastfeeding.
Conceiving a Baby and IUD
If you wish to conceive, a doctor or nurse can remove the IUD at any time, quickly restoring your fertility.
Can Women Without Children Get an IUD?
Absolutely. An IUD is not exclusive to women who have had children; it can be a suitable choice for anyone seeking effective contraception.
Can I Insert an IUD Myself?
No, self-insertion is not recommended. IUD insertion should be performed by a qualified healthcare provider or a doctor.
When Is the Best Time to Get an IUD Inserted? Is It Painful?
The ideal time for IUD insertion is immediately after menstruation or when you are certain you are not pregnant. The procedure itself, conducted in a doctor’s office, typically takes around five minutes. While some discomfort may be experienced during the internal examination, painkillers can help alleviate this sensation.
Post-Insertion: What to Expect?
After IUD insertion, some women may experience minor spotting or bleeding for a few days. This is generally nothing to worry about and is not usually heavy.
IUD as Emergency Contraception: A Highly Effective Option
IUDs can also serve as a form of emergency contraception after unprotected sex. They are even more effective than emergency contraceptive pills.
Dispelling Myths: Addressing Common Concerns
- IUD Migration: The risk of an IUD moving from the uterus to other parts of the body is extremely unlikely when properly placed.
- Spontaneous Expulsion: In rare cases, some women may naturally expel an IUD. Regular checks are essential to detect any issues.
- Early Removal: You can have an IUD removed at any time if desired, and the process is quick and simple.
Menstrual Changes with IUDs: Pain and Flow
IUDs can cause changes in menstrual patterns, including painful or heavier periods. These symptoms typically subside within a few months. Hormonal IUDs, in contrast, often lead to reduced menstrual flow.
Safety Considerations: Tampons and IUDs
Using tampons while an IUD is in place is safe and shouldn’t pose any risks.
Addressing Fertility, Cancer, and Sexual Comfort Concerns
- Fertility: IUD use does not impact fertility as it doesn’t inhibit ovulation or block the fallopian tubes.
- Cancer Risk: IUDs do not increase the risk of cancer.
- Sexual Comfort: IUDs are generally imperceptible during sex, ensuring a comfortable experience.
STI Protection
It’s crucial to note that IUDs do not provide protection against sexually transmitted infections (STIs). Practicing safe sex, such as using barrier methods (external or internal condoms) with new sexual partners remains essential, alongside preventing unintended pregnancies. Condoms can be used in conjunction with IUDs.
When to Remove IUD?
- Expiry Date: IUDs have an expiration date. When it’s past that date, it should be removed.
- Health Issues: If you develop a medical condition that doesn’t go well with the IUD, it should come out.
- Persistent Problems: If you’re having issues with the IUD that don’t get better, it may be time to take it out.
- Your Choice: And, of course, if you decide you want it out, that’s your call.
IUD Removal Procedure
To remove the IUD, your healthcare provider will gently grab the threads hanging down from your cervix using a special tool. They’ll pull it out carefully. If it doesn’t come out easily or hurts, they’ll figure out why before trying again. Sometimes, they might need to use a tiny camera to help remove it.
.