Pelvic Inflammatory Disease (PID) Symptoms, Treatment & Prevention
What is Pelvic Inflammatory Disease (PID) ?
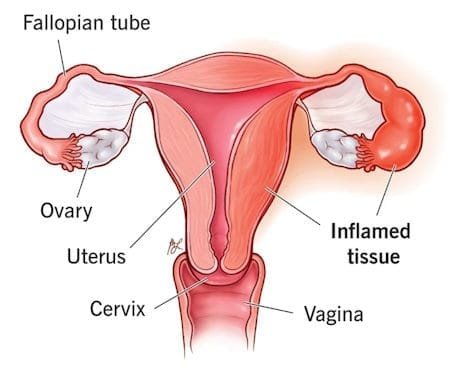
Pelvic inflammatory disease (PID) is a condition characterized by the infection of the female reproductive organs, including the uterus, fallopian tubes, and ovaries. It is primarily contracted through unsafe sexual practices and stands as one of the most severe consequences of sexually transmitted diseases (STDs). PID predominantly affects sexually active women aged 15 to 24 and can result in irreversible damage to the female reproductive system, ranking among the leading causes of infertility.
Types and Sites of Infection
PID can manifest as an infection in various parts of the female reproductive system, including:
- Cervix (cervicitis)
- Uterine lining (endometritis)
- Fallopian tubes (salpingitis)
- Ovaries (oophoritis)
- Area surrounding the ovaries and tubes (tubo-ovarian abscess)
- A combination of the above
Pelvic Inflammatory Disease, PID Risk Factors
PID affects approximately 5% of women in the United States, with a higher risk for those who:
- Have had a previous sexually transmitted infection (STI).
- Have previously experienced Pelvic Inflammatory Disease (PID).
- Are under 25 and sexually active (most common in women aged 15 to 24).
- Engage in sexual activity with multiple partners or a partner with multiple sexual partners.
- Practice douching, which can push bacteria into the reproductive organs and mask PID symptoms.
- Recently had an intrauterine device (IUD) inserted, with the highest PID risk occurring in the first few weeks post-insertion (rare after that), emphasizing the importance of STI testing before IUD placement.
- Have unsafe birthing experience.
- Have miscarriage or abortion, followed by infection.
PID can develop when the cervix is exposed to an STD, such as chlamydia or gonorrhea. In this scenario, the cervix loses its natural protective ability against bacteria, allowing the infection to progress to the uterus, ovaries, and fallopian tubes. Remarkably, a significant portion, ninety percent, of PID cases stem from untreated chlamydia and gonorrhea infections. Engaging in sexual practices involving multiple partners and unprotected sex substantially elevates the risk of acquiring STDs, which, in turn, can lead to the development of PID.
Pelvic Inflammatory Disease, PID Causes
PID typically results from bacteria in the vagina, with most cases being linked to sexual intercourse with a partner carrying a sexually transmitted infection (STI). Common STIs that cause PID include:
- Neisseria gonorrhoeae (causing gonorrhea)
- Chlamydia trachomatis (causing chlamydia)
- Mycoplasma genitalium
These bacteria usually start by infecting the cervix, causing cervicitis, and can subsequently ascend, leading to PID. PID is also more prevalent in women with bacterial vaginosis, where the overgrowth of normally residing vaginal bacteria can trigger symptoms and spread to other organs.
Less frequently, PID can occur following a vaginal delivery, abortion, or medical procedures such as dilation and curettage (D and C) or gynecologic surgery, introducing bacteria into the uterus. Douching also heightens the risk of infection.
Pelvic inflammatory disease, PID Symptoms
PID can show minor symptoms or no symptoms at all (common with chlamydial infection). Here are some common symptoms which may vary but can include:
- Dull pain in lower abdomen (tummy) and pelvis.
- Vaginal discharge that is green or yellow and often has a distinct and unpleasant odor.
- Pain during urination.
- Irregular menses.
- Fever or chills.
- Nausea, vomiting or diarrhea.
- Pain in the lower back.
- Discomfort or pain during sex that’s felt deep inside the pelvis.
Symptoms of PID usually emerge toward the end of the menstrual period or in the days following it. Women often experience mild to moderate lower abdominal pain, which may be more pronounced on one side. Other indicators include irregular vaginal bleeding and vaginal discharge, sometimes accompanied by an unpleasant odor.
As the infection progresses, lower abdominal pain intensifies, possibly accompanied by a mild fever (usually below 102°F or 38.9°C), nausea, or vomiting. Fever may subsequently increase, and the discharge may become pus-like and yellow-green. Some women may also endure discomfort during sexual intercourse or urination.
Notably, while the infection can be severe, it might cause mild or no symptoms. Symptoms attributed to gonorrhea are generally more severe than those of chlamydia or infections caused by Mycoplasma genitalium, which may remain asymptomatic without noticeable discharge or symptoms.
If you notice these symptoms, it is important to stop having intercourse and visit your doctor immediately, as prompt treatment is vital for PID.
Complications of Pelvic Inflammatory Disease, PID
Pelvic inflammatory disease (PID) can lead to various complications, including:
- Blocked Fallopian Tubes: PID may result in the blockage of the fallopian tubes. This blockage can cause the tubes to swell due to trapped fluid, resulting in pressure and chronic lower abdominal pain.
- Peritonitis: In severe cases, the infection can spread to the membrane lining the abdominal cavity, causing peritonitis. This condition leads to sudden or gradual severe abdominal pain throughout the abdomen.
- Fitz-Hugh-Curtis Syndrome: When PID, caused by gonorrhea or chlamydia, extends to the tissues around the liver, it can trigger Fitz-Hugh-Curtis syndrome. Adhesions form between the Liver and the peritoneum. This condition manifests as pain in the upper right side of the abdomen, resembling the symptoms of gallbladder disorders or gallstones.
- Abscess Formation: In about 15% of women with infected fallopian tubes, abscesses may develop, particularly in cases of prolonged infection. If an abscess ruptures, pus can spill into the pelvic cavity, leading to peritonitis. A rupture causes severe lower abdominal pain, followed rapidly by nausea, vomiting, and a significant drop in blood pressure, which is indicative of shock. In some instances, the infection may enter the bloodstream, a condition known as sepsis, which can be life-threatening and constitutes a medical emergency.
- Adhesions: PID can induce the formation of abnormal scar tissue bands known as adhesions. These bands can develop when PID generates pus-like fluid, irritating tissues and causing scar tissue to form within reproductive organs or between abdominal organs. This scarring and adhesions can result in infertility and chronic pelvic pain. The risk of these complications increases with the severity and recurrence of inflammation.
- Tubal Pregnancy (Ectopic Pregnancy): Women with a history of PID are 6 to 10 times more likely to experience a tubal pregnancy, a type of ectopic pregnancy. In tubal pregnancies, the embryo develops in a fallopian tube rather than the uterus, posing a life-threatening risk to the woman, with the fetus unable to survive.
- Infertility: PID is a leading cause of preventable infertility in the United States .When PID is left untreated, it can result in scarring and the formation of abscesses (infected fluid) in the fallopian tubes thus leading to infertility. Scarring caused by PID can block the fallopian tubes, hindering egg transport to the uterus. This scarring may necessitate fertility treatments for conception. Approximately 1 in 10 women with PID may become infertile due to the condition, especially those who experience delayed treatment or recurrent episodes of PID.
Pelvic Inflammatory Disease, PID Diagnosis
PID is typically diagnosed through the following methods:
- Doctor’s Evaluation: Doctors suspect PID if women exhibit lower abdominal pain or unexplained vaginal discharge, especially within childbearing age or in the presence of purulent discharge. A thorough physical examination, including a pelvic exam, is performed. Pelvic pain during the examination supports the diagnosis.
- Cervical Sample Analysis: A sample is commonly obtained from the cervix using a cotton swab and tested to detect gonorrhea or chlamydia. Even if these tests yield negative results, PID may still be present.
- Ultrasonography: Pelvic ultrasound may be employed if pain hinders a comprehensive physical examination or if further information is required. Ultrasonography can identify abscesses in the fallopian tubes or ovaries, as well as tubal pregnancies.
- Pregnancy Test: A pregnancy test may be conducted to rule out the possibility of a tubal pregnancy, a potential cause of the symptoms. Additional symptoms and laboratory findings assist in confirming the diagnosis.
- Laparoscopy: In cases where the diagnosis remains uncertain or when a woman does not respond to treatment, a viewing tube called a laparoscope may be inserted through a small incision near the navel. This procedure allows doctors to inspect the abdominal interior and obtain fluid samples for testing. It can definitively confirm or rule out PID.
Pelvic inflammatory disease, PID Treatment
PID is treated primarily with antibiotics ,often a combination of two antibiotics effective against various bacteria.. Prompt treatment is essential to prevent severe complications. Antibiotics for gonorrhea and chlamydia are typically administered orally or via intramuscular injection. These antibiotics are usually initiated as soon as possible and may be modified based on subsequent test results. Completing the entire antibiotic course is crucial, even if symptoms improve. A follow-up with a healthcare provider after 2-3 days ensures the antibiotics are working.
In cases where hospitalization is required, such as when the infection persists beyond 72 hours, when the woman experiences severe symptoms or a high fever, when she is pregnant, when an abscess is suspected, when vomiting prevents oral antibiotic intake at home, or when the diagnosis remains uncertain, antibiotics are administered intravenously in a hospital setting.
Abscesses that do not respond to antibiotic therapy may necessitate drainage. This is often performed using a needle, which is inserted through a small incision in the skin, guided by imaging tests like ultrasonography or computed tomography (CT). A ruptured abscess is considered a medical emergency, characterized by severe lower abdominal pain followed by nausea, vomiting, and a significant drop in blood pressure. Surgery may be considered if symptoms persist or if abscesses do not resolve.
Women are advised to abstain from sexual activity until they have completed their antibiotic treatment and a doctor confirms the complete elimination of the infection, even if their symptoms have resolved. Additionally, all recent sexual partners should be tested for gonorrhea and chlamydia and, if necessary, treated. With prompt diagnosis and treatment, most women recover fully.
Prevention of Pelvic Inflammatory Disease (PID)
The best approach to PID is prevention:
- Avoid unsafe sexual practices and having multiple sexual partners. Use barrier methods like condoms and spermicides.
- If you have multiple sexual partners, consider avoiding the use of an intrauterine device (IUD).
- Be vigilant for symptoms and seek prompt treatment if you notice any.
- Maintain regular follow-ups with your doctor to identify and prevent early-stage infections from spreading to your reproductive organs.
- Avoid douching, as it disrupts the delicate balance of bacteria in your vagina, masks vaginal discharge, and can push bacteria into the genital tract.










